Effect of healthy lifestyle on lipid profile in a young woman with overweight
Pusadee Luenee, Noppadol Arechep, Sudcharee Kiartivich and Kosit Sribhen
Department of Clinical Pathology, Faculty of Medicine Siriraj Hospital,
Mahidol University, Bangkok, Thailand
Correspondence to:
Dr Kosit Sribhen,
Department of Clinical Pathology, Floor 10, Adulyadejvikrom Building,
Faculty of Medicine Siriraj Hospital, Mahidol University,
2 Wanglang Road, Bangkoknoi, Bangkok, 10700 Thailand.
Telephone: +66 (0) 2 419 6587 – 9 Fax: +66 (0) 2 418 1367 Email: chos_kos@hotmail.com
Conflict of interest: The authors declare that they have no conflicts of interest with the contents of this article.
Abstract
In the past decades, the prevalence of overweight and obesity have increased substantially worldwide, especially in South-East Asia countries including Thailand. Recent data from prospective studies have indicated that overweight and obesity in children and adolescents are predictors of adult obesity. There is also substantial evidence that the association between obesity and cardiovascular disease is explained by the adverse cardiovascular risk factor profile including hypertension, type 2 diabetes mellitus and dyslipidaemia. Since the occurrence of overweight and obesity is mainly attributed to an unhealthy lifestyle (unhealthy diet and sedentary behaviour), we demonstrated in a case study that adopting a lifestyle of consuming a healthy diet and performing regular physical activity can reverse the adverse abnormal lipid profile seen in our overweight patient.
Keywords: healthy lifestyle; lipid profile; overweight
Introduction
Increased serum concentrations of total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) represent established major cardiovascular disease (CVD) risk factors, and LDL-C levels have long been used as the target for lipid-lowering therapy. The role of triglycerides (TG) in predicting cardiovascular risk, on the other hand, is the topic of debate for several decades. Recent data from prospective epidemiological and genetic studies have, however, indicated that TG and TG-rich lipoprotein including remnant cholesterol (RN-C) have a causal association with the development of atherosclerotic cardiovascular disease (ASCVD)(1,2). We report herein a case of a young women with overweight, in whom adoption of a healthy lifestyle alone, without the use of lipid-lowering medication, resulted in a significant improvement in serum lipid profile.
Case Report
A 27-year-old woman came to the hospital because she was concerned about her abnormal lipid profile detected at the routine laboratory check-up in the year 2017. She reported to have no family history of hypercholesterolaemia or dyslipidaemia associated with type 2 diabetes mellitus. Her calculated body mass index (BMI) was high at 25.6 kg/m2, indicating an overweight(3), and her waist circumference was normal at 78 cm. Laboratory investigations of liver and renal function as well as plasma glucose were all in the normal ranges.
Serum concentrations of lipid and lipoprotein were determined on a fully-automated analyzer Cobas 602 (Roche Diagnostics) using standard enzymatic methods. As shown in Table, serum TG (reference value < 150 mg/dL) and high-density lipoprotein cholesterol (HDL-C, reference value > 50 mg/dL) level was high and low at 304 mg/dL and 41 mg/dL, respectively, resulting in a high TG to HDL-C ratio of 7.41. The calculated RN-C (TC minus LDL-C minus HDL-C, reference value < 30 mg/dL) level was also high at 61 mg/dL. Her TC, LDL-C (calculated by Friedewald formula: LDL-C = TC – HDL-C – TG/5), and non-HDL-C (TC minus HDL-C, reference value < 200, 130 and 160 mg/dL, respectively) levels in 2017 were all above the reference ranges. A retrospective analysis of the data between the year 2014 and 2017 has revealed a rising trend in serum levels of TG and RN-C, and a decreasing trend in concentrations of HDL-C. A rising trend in levels of TC, LDL-C and non-HDL-C was also observed (Table).
Table: Serum lipid and lipoprotein concentrations serially determined between the year 2014 and 2019.
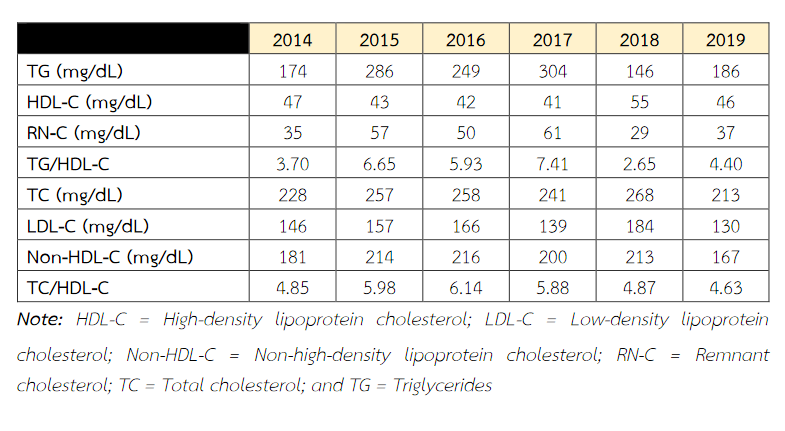
Based on these results, the patient was advised to adopting a healthy lifestyle which primarily consists of a healthy diet (increase consumption of fruits, vegetables and fish, and reduce intake of fatty and high sodium foods as well as sugar-sweetened beverages) and regular physical activity (150 minutes/week of moderate-intensity leisure-time activity). As can be seen in Table, there was a significant improvement in the dyslipidaemic profile, with a marked decrease in TG level to the reference range, and a significant rise in HDL-C level, resulting in a low TG/HDL-C ratio after one year of intervention. The RN-C level also showed a decline toward the reference range. Although a rising trend in TG and RN-C concentrations, and a decreasing trend in HDL-C levels were seen after 2 years of intervention (in 2019) as compared with those in 2018, they still showed a favourable profile compared to those before intervention in the year 2017. In contrast, an increasing trend in TC, LDL-C and Non-HDL-C levels, measured in 2018, compared to those determined in 2017 was observed. Nevertheless, their concentrations in 2019 exhibited a strong favourable lipid profile compared to all of those determined between the year 2014 and 2018. Of interest is the observation that all of the lipid and lipoprotein levels determined in 2019 were comparable to those measured in 2014 (Table). In this context, it is important to note that during the 2-year period of intervention, her BMI and waist circumference have declined from 25.6 to 24.0 kg/m2 and 78 to 74 cm, respectively.
Discussions
The main findings in the present case study are that adoption of a healthy lifestyle alone, without the need for pharmacologic intervention, results in a significant increase in HDL-C serum concentration and a considerable reduction in TG level and the TG/HDL-C ratio. Since all the lipid parameters mentioned above have been proved to be strong predictors of ASCVD(4,5), their measurements should be routinely used, along with those of TC and LDL-C, in the risk assessment of cardiovascular disease. In addition, calculation of RN-C level should be performed to predict residual cardiovascular risk, especially in patients with overweight or obese, since this novel parameter has recently been shown to be a potent atherogenic lipoprotein similar to that of LDL-C(6,7). Recently, calculated RN-C has been recommended to be used as an optional parameter in addition to the standard lipid profile (TC, TG, HDL-C, LDL-C and Non-HDL-C) for cardiovascular risk assessment(8). In this context, it has been reported that a healthy diet alone may not represent a useful tool to significantly reduce serum TC and LDL-C concentrations. According to the US National Cholesterol Education Programme, Step I or Step II diet lead only to a 12% and 16% reduction in LDL-C level(9), respectively, a far less lipid-lowering effect compared to the effect of lipid-lowering drug in the statin group of 30 to 50%. However, it has been recommended that the use of statins in primary prevention should be confined to the patients considered to be at intermediate or high risk of developing cardiovascular disease(10,11). On the other hand, by considering the young age and the absence of major CVD risk factors (smoking, hypertension and diabetes mellitus), our patient can be classified into the low risk group in which there is no indication for pharmacological treatment. Nonetheless, the data from this case report indicated that the use of the combination of a healthy diet and regular physical activity can result in a significant reduction in atherogenic lipid and lipoprotein levels. Similar observations have been made in several recent studies on children and adolescents(12,13), as well as in adults(14).
Conclusion
It can be concluded that performing a lifelong healthy lifestyle may represent the appropriate treatment modality in this patient.
References
- Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet 2014; 284: 626-35.
- Khera AV, Kathiresan S. Genetics of coronary artery disease: discovery, biology and clinical translation. Nat Rev Genet 2017; 18: 331-44.
- WHO Expert Consultation. Appropriate body mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157-63.
- Prasad M, Sara J, Widmer RJ, Lennon R, Lerman LO, Lerman A. Triglyceride and triglyceride/HDL (high density lipoprotein) ratio predict major adverse cardiovascular outcomes in women with non-obstructive coronary artery disease. J Am Heart Assoc 2019; 8: e009442.
- Vallejo-Vaz AJ, Fayyad R, Boekholdt SM, Hovingh GK, Kastelein JJ, Melamed S, et al. Triglyceride-rich lipoprotein cholesterol and risk of cardiovascular events among patients receiving statin therapy in the TNT Trial. Circulation 2018; 138: 770-81.
- Nakajima K, Tanaka A. Atherogenic postprandial remnant lipoprotein; VLDL remnants as a causal factor in atherosclerosis. Clin Chim Acta 2018; 478: 200-15.
- Varbo A, Benn M, Tybjaerg-Hansen A, Jorgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol 2013; 61: 427-36.
- Langlois MR, Nordestgaard BG, Langsted A, Chapman J, Aakre KM, Baum H, et al. for the European Atherosclerosis Society (EAS) and the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) Joint Consensus Initiative. Quantifying atherogenic lipoproteins for lipid-lowering strategies: consensus-based recommendations from EAS and EFLM. Clin Chem Lab Med 2019, doi.org/10.1515/cclm-2019-1253.
- Yu-Poth S, Zhao G, Etherton T, Naglak M, Jonnalagadda S, Kris-Etherton PM. Effects of the National Cholesterol Education program's step I and step II dietary intervention programs on cardiovascular disease risk factors: a meta-analysis. Am J Clin Nutr 1999; 69: 632-46.
- Michos ED, McEvoy JW, Blumenthal RS. Lipid management for the prevention of atherosclerotic cardiovascular disease. N Engl J Med 2019; 381: 1557-67.
- Anderson TJ, Gregoire J, Pearson GJ, Barry AR, Conture P, Dawes M., et al. 2016 Canadian Cardiovascular Society Guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Canadian J Cardiol 2016; 32: 1263-82.
- Kim SH, Song YH, Park S, Park MJ. Impact of lifestyle factors on trends in lipid profiles among Korean adolescents: the Korea National Health and Nutrition Examination Surveys study, 1998 and 2010. Korean J Pediatr 2016; 59: 65-73.
- Cugnetto ML, Saab PG, Llabre MM, Goldberg R, McCalla JR, Schneiderman N. Lifestyle factors, body mass index and lipid profile in adolescents. J Pedriatr Psychol 2008; 33: 761-71.
- Chitra U, Reddy NK, Balakrishna N. Role of lifestyle variables on the lipid profile of selected South Indian subjects. Indian Heart J 2012; 64: 28-34.


