Rhinosporidiosis of maxillary sinus: an unusual site – a case report
Rhuta Shah
Excellence Diagnostic Pathlab, Shop number 108, First Floor, c/o Sarvar Clinic,
Above Geeta Khaman House, Vruj Bhoomi Complex, Chala, VAPI-396191,
Taluka-Vapi, Valsad, Gujarat, India.
Telephone: +91 942 815 9081 Email: dr.rhutashah@gmail.com
Conflict of interest: The author declares that he/she has no conflicts of interest with the contents of this article.
Abstract
Rhinosporidiosis, a rare form of fungal sinusitis usually affects nasal mucosa with mass forming lesion mimicking nasal polyp. Here we present a case of rhinosporidiosis at very unusual location – primarily affecting maxillary sinus, presenting as nasal polyp and causing bony erosion of maxilla. Thus fungal sinusitis should be kept in mind as differential diagnosis in case of sinonasal mass lesion.
Keywords: maxillary sinus; polyp; rhinosporidiosis
Introduction
Rhinosporidiosis is a rare and chronic infestation caused by fungus Rhinosporidium seeberi, seen in India and Sri Lanka and is hyperendemic in southern parts of Tamil Nadu. It predominantly affects mucus membrane of nose and nasopharynx causing polypoidal growth(1). We report of a case of Rhinosporidiosis presenting as nasal polyp and affecting maxillary sinus. Caldwell-Luc operation was performed.
Case Report
A 32-year-old female patient came to the outpatient department of Otorhinolaryngology with complaint of nasal obstruction since 1 year. She has recurrent episodes of nasal blockage and rhinorrhoea since 1 year. There was no history of otalgia, epistaxis or no other contributing medical history. Anterior rhinoscopy revealed pinkish polypoidal yet friable looking mass filling right nasal cavity. Nasal mucosa was swollen, congested with non-pulsatile, non-expansile polyp like mass with it. X-ray examination of the paranasal sinuses showed haziness of maxillary sinus on right side with soft tissue mass in right nasal cavity. A differential diagnosis of polyp, cholesteatoma, fungal infection of maxillary sinus was put forward. Caldwell-Luc operation was performed and parts of polypoidal growth, affected mucosa and cheesy looking material was removed and all of these tissues were sent for histopathology.
Specimen received consisted of multiple soft tissue pieces, collectively measuring 3.5 x 3 x 1 cm. On gross examination, fragmented parts of polyp with irregular/nodular surface, tense shiny white mucosa, and yellowish white friable cheesy material was seen (Figure 1). Polyp and mucosal tissue fragments also showed such yellow white spots on its surface. Haematoxylin and eosin (H&E) – stained section showed polyp fragments covered by respiratory epithelium with densely inflamed vascular connective tissue in its substance (Figure 2). There was abundant amount of pinkish friable looking necrosis. Bony spicules with attached epithelium representing bony erosion were also seen. The necrotic areas had numerous birefringent thick-walled sporangia containing numerous "endospores (daughter spores)" in different stages of development. These histological findings were characteristics of rhinosporidiosis (Figures 3 – 4).
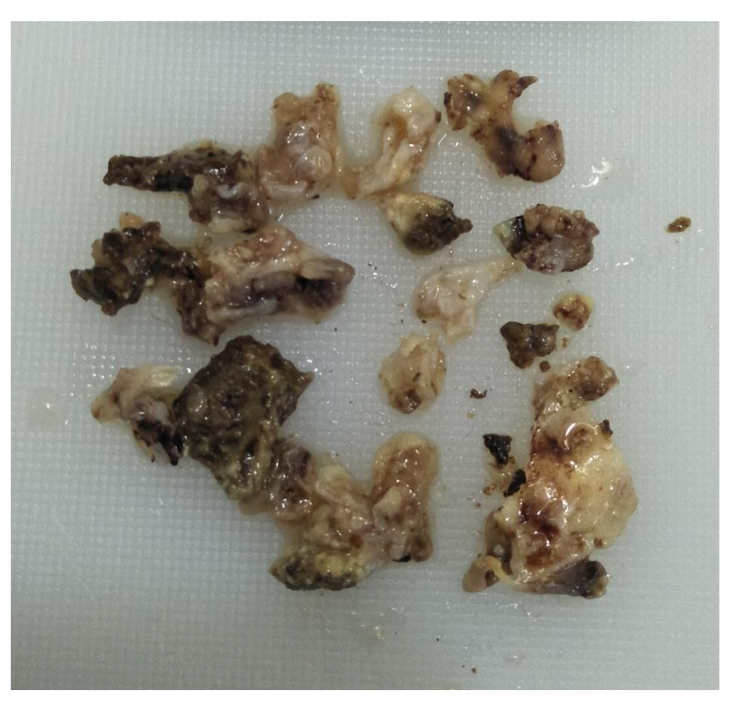
Figure 1 Multiple polyp fragments with tense shiny mucosal wall, irregular nodular looking surface and cheesy material.
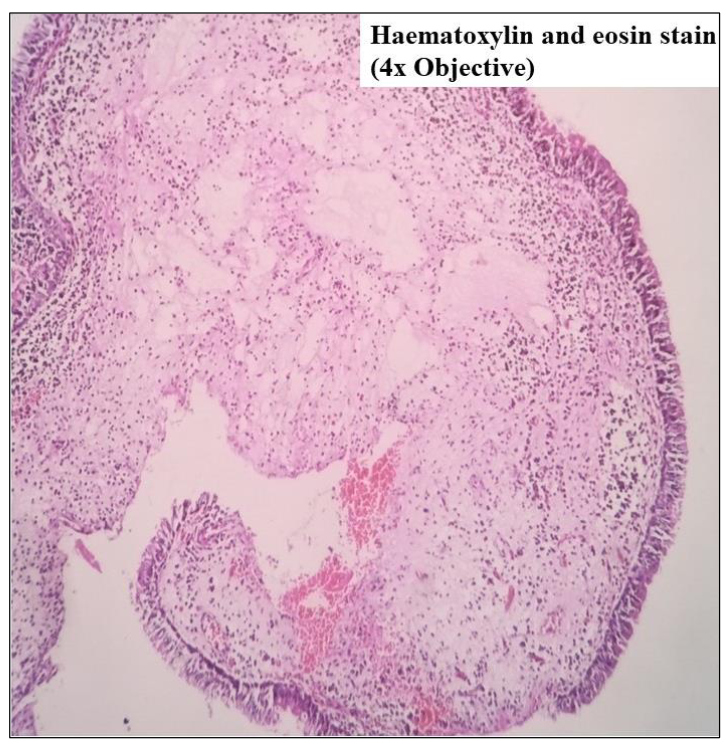
Figure 2 Polyp fragment lined by respiratory epithelium and densely inflamed fibrovascular connective tissue in its substance.
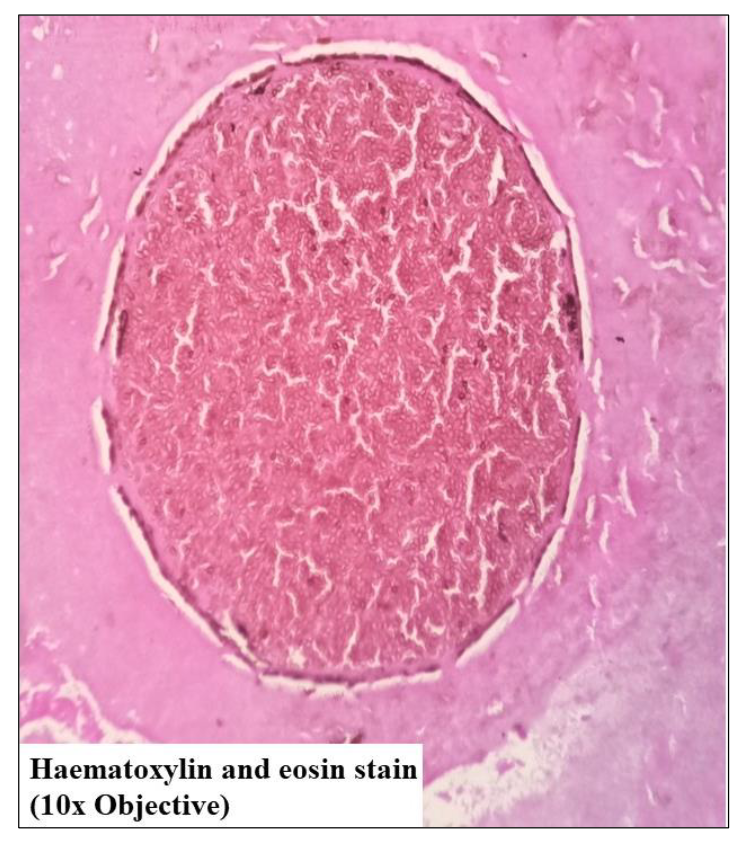
Figure 3 Large thick-walled sporangium with numerous endospores within it.
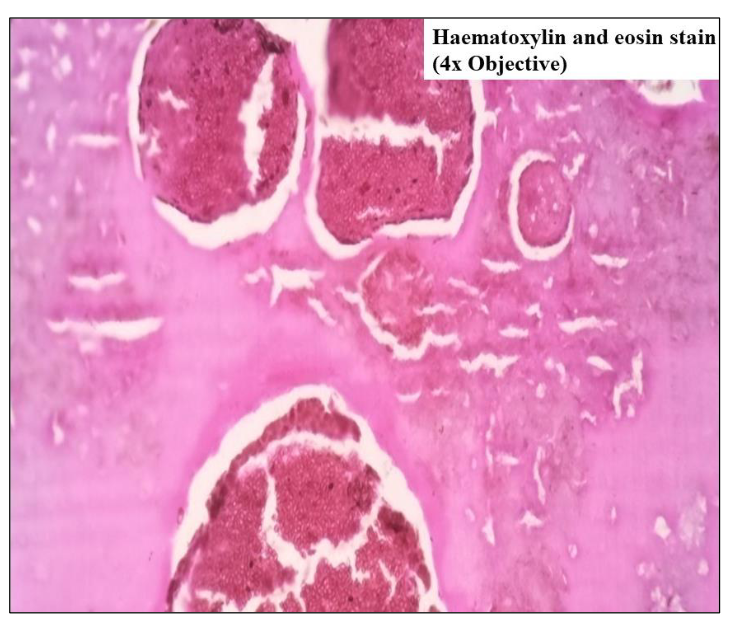
Figure 4 Numerous sporangia with daughter spores surrounded by pinkish fibrillary necrotic material.
Discussions
Rhinosporidiosis is a chronic infectious granulomatous disease of the upper respiratory tract characterised by the formation of polypoid masses(2). It affects all ages but is most common in the third and fourth decades. The most common sites are nasal mucosa, nasopharynx, oropharynx and nasolacrimal duct. The most common symptoms are nasal obstruction, epistaxis, and rhinorrhoea. Other sites of involvement may include the larynx, tracheobronchial tree, oesophagus, conjunctiva and ears.
Habitual bathing in rivers and ponds has been strongly associated with rhinosporidiosis(3). Water and soil are believed to be the reservoir of infection, given the increased incidence of disease found in sand workers, paddy cultivators, and people bathing in stagnant muddy waters. Mode of transmission is through water or dust, from which the endospores penetrate the nasal mucosa, mature into sporangium within the submucosal compartment, and after maturation burst with release of sporangia into surrounding tissue.
The biological agent has a mature stage that consists of large, thick-walled spherical structures (called sporangia) containing smaller "daughter cells (called sporangiospores or endospores)"(4). Sporangia containing innumerable endospores seen with haematoxylin and eosin stain; organisms also stain with periodic acid–Schiff, mucicarmine and Gomori methenamine silver stains(2,4). Since it is primarily a disease affecting the orofacial region, it is of great value to the oral physician, oral radiologist and oral surgeon, and a necessary differential to be kept in mind for sinonasal masses. As all attempt to cultivate the causative organism in vitro has been unsuccessful, the diagnosis depends on clinical and histopathological findings(2,5).
Surgical excision is the mainstay of treatment. It has been advocated that a wide surgical margin is necessary to reduce the risk of recurrence, though this may be associated with significant morbidity like haemorrhage and nasal septal perforation. Because of this, limited surgical excision with cautery of the base of the lesion has been attempted, and to further reduce the risk of recurrence(4).
Systemic dapsone therapy is used as an adjunct to surgical intervention and helps in preventing recurrences in immunocompetent patients and is known to prevent recurrence by arresting the maturation of sporangia and promoting fibrosis in adjacent tissues(4).
Conclusions
The rhinosporidiosis must be taken as a differential diagnosis of the nasal polypoid lesions or sinonasal mass. The intranasal lesions must always be evaluated with details, by making a critical anamnesis and always considering the patient's origin. Histopathological examination is necessary to find out aetiological factor(6).
References
- Kindo AJ, Kalyani J, Sundaram S, Senthil KM, Kumar AR. Unusual presentation of rhinosporidiosis – a case report. Sri Ramachandra Journal of Medicine 2007;1(2):60-1.
- Kazi AZ, Kazi HZ, Channe RC, Kulkarni AS. Rhinosporidiosis of maxillary sinus: a case report. Journal of Indian Academy of Oral Medicine and Radiology 2019;31(3):274.
- Weidner N, Cote RJ, Suster S, Weiss LM. Modern Surgical Pathology E-Book. Elsevier Health Sciences, 2009:189.
- Babu S, Anuradha A, Chandra S, Kashyap B. Rhinosporidiosis: a case report with review of literature. Ann Trop Med Public Health 2012;5:127-9.
- Thompson LD. Head and Neck Pathology E-book: A Volume in the Series: Foundations in Diagnostic Pathology. Elsevier Health Sciences, 2012.
- Crosara PFTB, Becker CG, Freitas VA, Nunes FB, Becker HMG, Guimarães RES, et al. Nasal rhinosporidiosis: differential diagnosis of fungal sinusitis and inverted papilloma. Int Arch Otorhinolaryngol. 2009;13(1):93-95.


