Low-Grade Central Osteosarcoma of Ilium, A Case Report.
Artit Jinawath1 , Saran Subhadrabandhu2 , Suphaneewan Jaovisidha3 ,
Vorachai Sirikulchayanonta4
1 Department of pathology, Ramathibodi hospital, Mahidol University, Bangkok, Thailand.
2 Department of orthopaedics, Ramathibodi hospital, Mahidol University, Bangkok, Thailand.
3 Department of radiology, Ramathibodi hospital, Mahidol University, Bangkok, Thailand.
4Faculty of Science, Rangsit University, Pathumthani 12000, Thailand.
Corresponding author: Artit Jinawath
Department of pathology, Ramathibodi hospital, Mahidol University, Bangkok, Thailand
Email: artitjp@yahoo.com
Received 7th August 2016; Accepted 7th October 2016
Abstract
Low-grade central osteosarcoma accounts for 1-2% of all osteosarcomas, and is usually found in long bones of extremities. To our best knowledge, low-grade central osteosarcoma of pelvic bone is unusually rare. We report a case of low-grade central osteosarcoma in the ilium of a 36-year-old man. Our case appears to be the first well-illustrated imagings for this location. Differential diagnosis includes fibrous dysplasia and conventional fibroblastic type osteosarcoma. The awareness of this entity should lead to avoid over or under treatment.
Keywords: Low grade central osteosarcoma, ilium, immunohistochemistry, magnetic resonance imaging.
Introduction
Low grade central osteosarcoma (LGCO) is a rare subtype of osteosarcoma which represents 1-2% of osteosarcomas (1). This tumor usually affects the long bones, especially distal tibia and proximal femur in the age group between second and third decades (1). LGCO can mimic benign lesions on the plain radiographs (2, 3, 4). The prognosis of LGCO is much better than conventional type high grade osteosarcoma with 5 years survival more than 90% of cases (1, 5). To our best knowledge, LGCO involving pelvic bones is rather unusual. We therefore report a case involving ilial bone which appears to be the first case at this location of which comprehensive imaging studies were performed.
Case presentation
A 36-year-old male had developed pain in the left pelvic area one year prior to observing a slow-growing mass at this location which lasted for almost two years. Physical examination revealed ill-defined mass at left hip area. No gait deficit was detected. Plain radiograph revealed a large permeative mixed osteolytic-osteoblastic lesion involving peripheral half of the left iliac wing with cortical breakthrough and hair-on-end periosteal reaction (figure 1). 99mTc bone scintigraphy revealed strong radioisotope uptake in the entire left ilium extending down to the left acetabulum (figure 2). The magnetic resonance imaging (MRI) showed a marrow-replacing lesion at the left ilium with cortical destruction, sunray periosteal reaction, along with a large accompanying soft tissue mass. The lesion extended down to involve the continuing acetabulum (figure 3, 4). CT scan (figure 4 C) disclosed osteoid matrix within the mass. All findings were suggestive of osteosarcoma. Plain radiographs and CT of the chest revealed absence of metastasis. The open biopsy was performed and the initial diagnosis was conventional osteosarcoma, fibroblastic type. However, this case was reviewed thoroughly and the diagnosis was changed to LGCO. The tumor was removed by internal hemipelvectomy of left pelvic bone. The margins of resection were reportedly free of lesion by histologic examination. The radiographs of the resected specimen were shown on figure 5. The gross specimen showed a well-defined white solid mass measuring 16x12x9 cm enmeshed in the nearby skeletal soft tissue (figure 6). The histology of both biopsy- and resected specimens revealed well trabeculated woven bones surrounded by cellular spindle cells having mildly atypical hyperchromatic nuclei and occasional mitotic activity (figure 7A and 7B). Neither high grade nor dedifferentiated foci were detected. Immunostains using anti-MDM2 and CDK4 antibodies demonstrated positive nuclear stainings (figure 8A and 8B), supporting the diagnosis of LGCO (6). After surgery he was referred to the registered provincial hospital for follow-up. Recently we have been verbally acknowledged that he developed pulmonary metastasis. No information regarding recurrence of this tumor was known.

Figure 1. A large mixed osteolytic and osteosclerotic lesion involved peripheral half of the left iliac wing that breaking through cortex with hair-on-end periosteal reaction and a wide area of cloud-like osteoid matrix.
Discussion
LGCO is a less aggressive type of osteosarcoma predominantly arising in long bones with limited potential for distant metastasis (1, 5). Marginal excision often resulted in local recurrence (1, 5). Wide excision with adequate margin provided low chance of local recurrence (1, 5). Many reports mentioned that recurrent tumors often transform to a higher-grade osteosarcoma (dedifferentiated LGCO) and possess higher metastatic potential (1, 4, 5, 6). Chemotherapy (neoadjuvant or adjuvant regimens) and radiotherapy did not appear to have substantial benefit in the treatment of LGCO (1, 4, 5, 6, 8). To our best knowledge, low grade osteosarcoma of pelvic bones was rarely reported in the literature (2, 7), our case appears to be the first comprehensive imaging illustrations for this particular site.
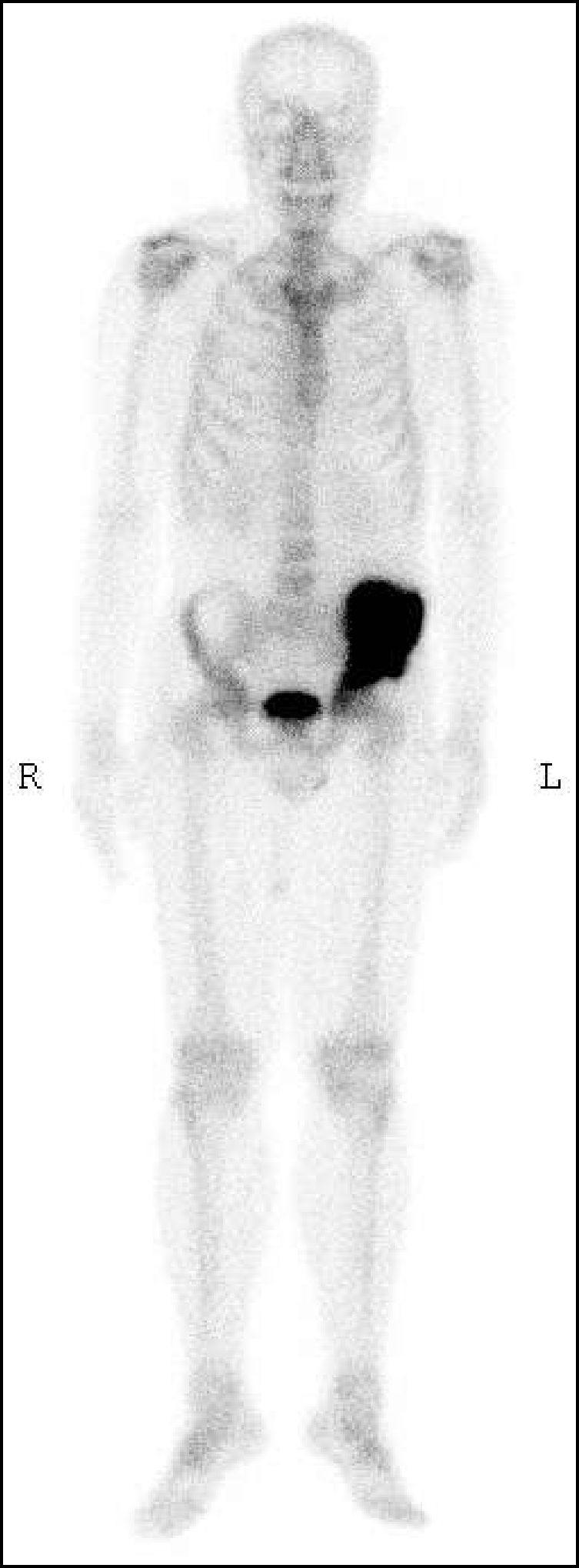
Figure 2. 99mTc Bone scan revealed intense radioisotope uptake in the entire left ilium continuing to the left acetabulum.
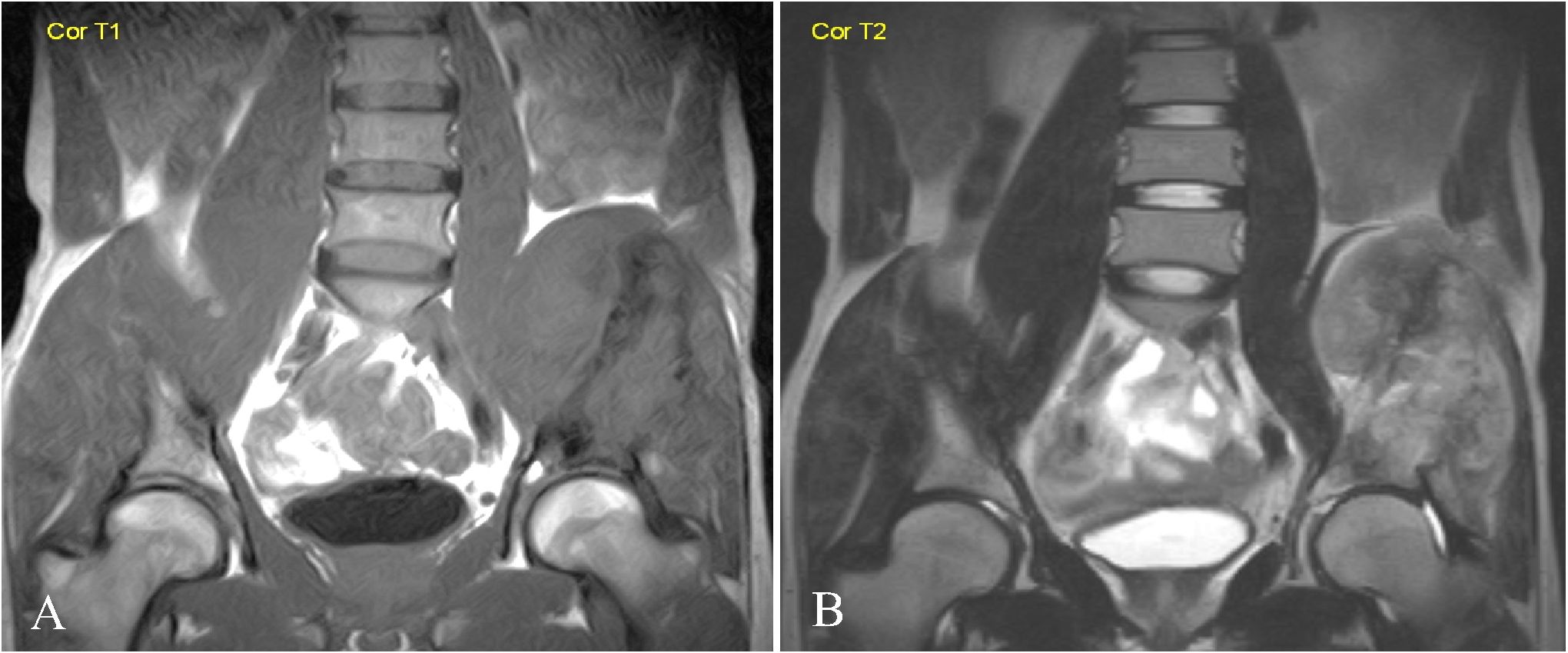
Figure 3. Coronal MR images on Tl-weighted (A) and T2-weighted with fat suppression (B) sequences revealed bone destruction of the left ilium accompanied by a large soft tissue component. No definite involvement of the left hip joint was demonstrated.
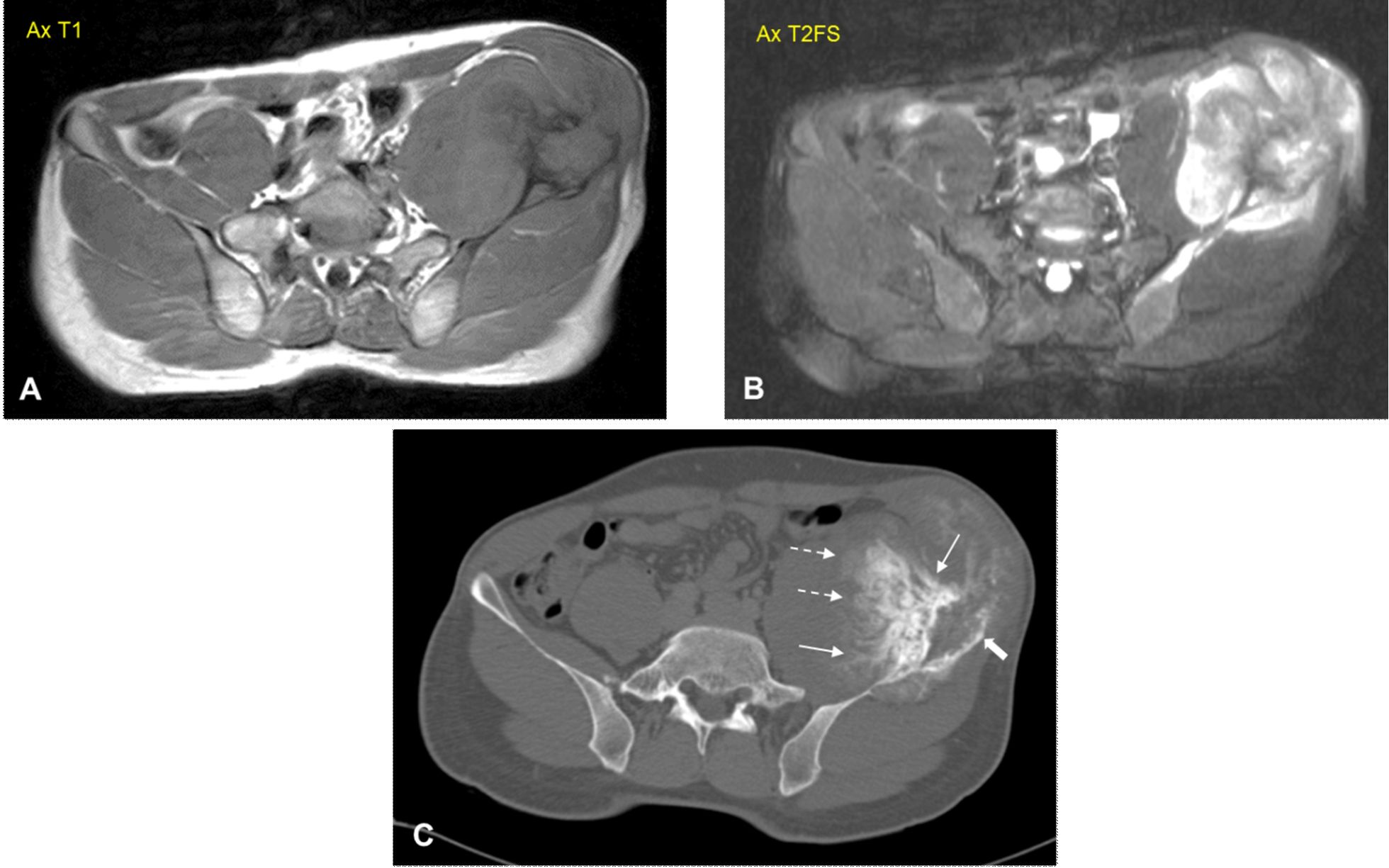
Figure 4. Axial MR images on T1-weighted (A) and T2-weighted with fat suppression sequences (B), and MDCT scan viewing in bone window (C). In (C) there was a pattern of osteolytic-osteosclerotic expanding lesion (thick white arrow) involving the left iliac wing with hair-on-end periosteal reaction (thin white arrows) and cloud-like osteoid matrix (dotted white arrows). Soft tissue component was obviously seen by MR images. All findings were suggestive of osteosarcoma.
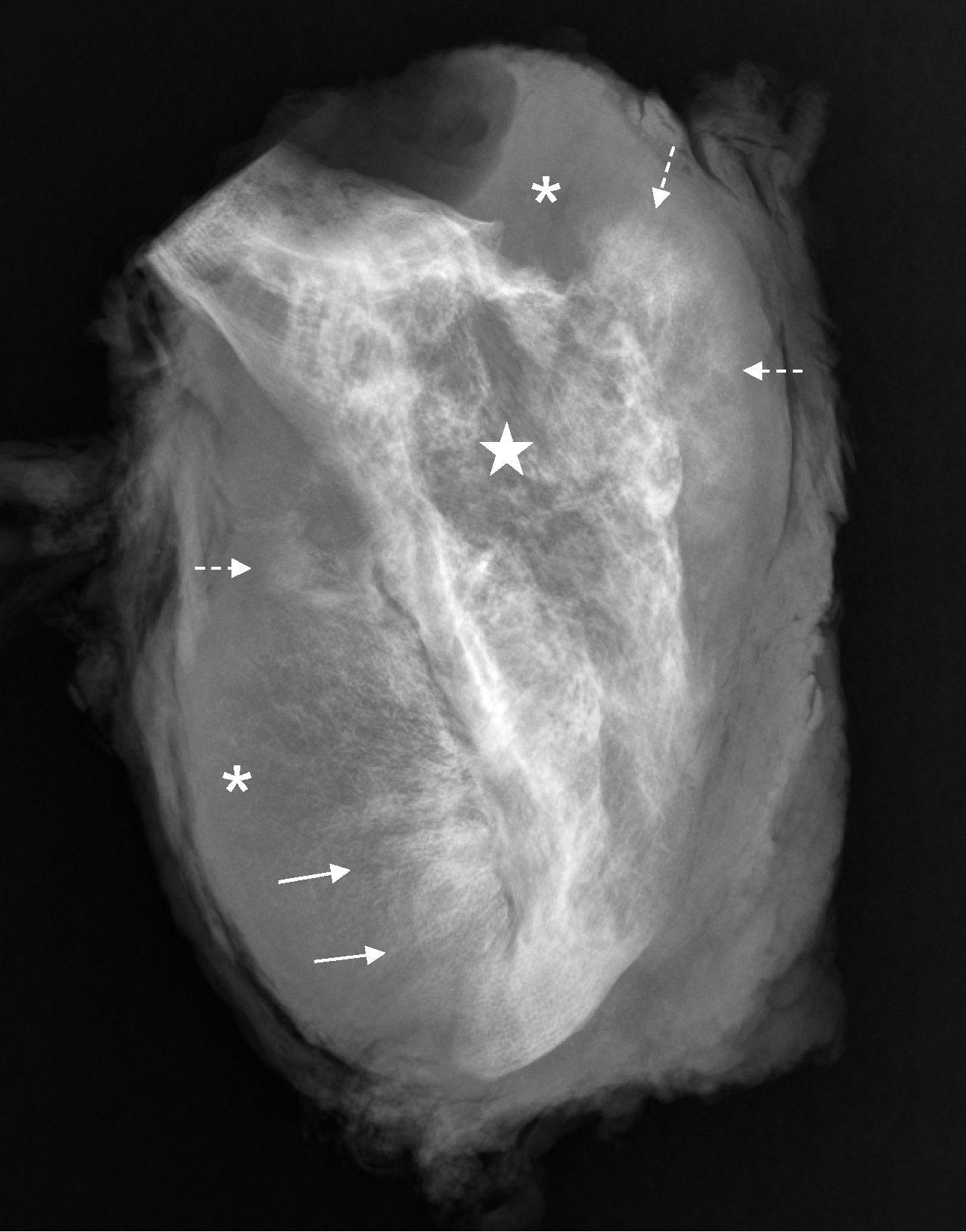
Figure 5. Specimen radiograph of the resected left ilium confirmed the osteolytic expanding lesion (white star) involving the left iliac wing with hair-on-end periosteal reaction (thin white arrows) and cloud-like osteoid matrix (dotted white arrows). Soft tissue component was obviously seen as well (asterisks).

Figure 6. The cut surface of the left hemipelvectomy specimen showed well circumscribed firm white extraosseous mass measuring 16x12x9 cm. locating in the surrounded skeletal muscle.
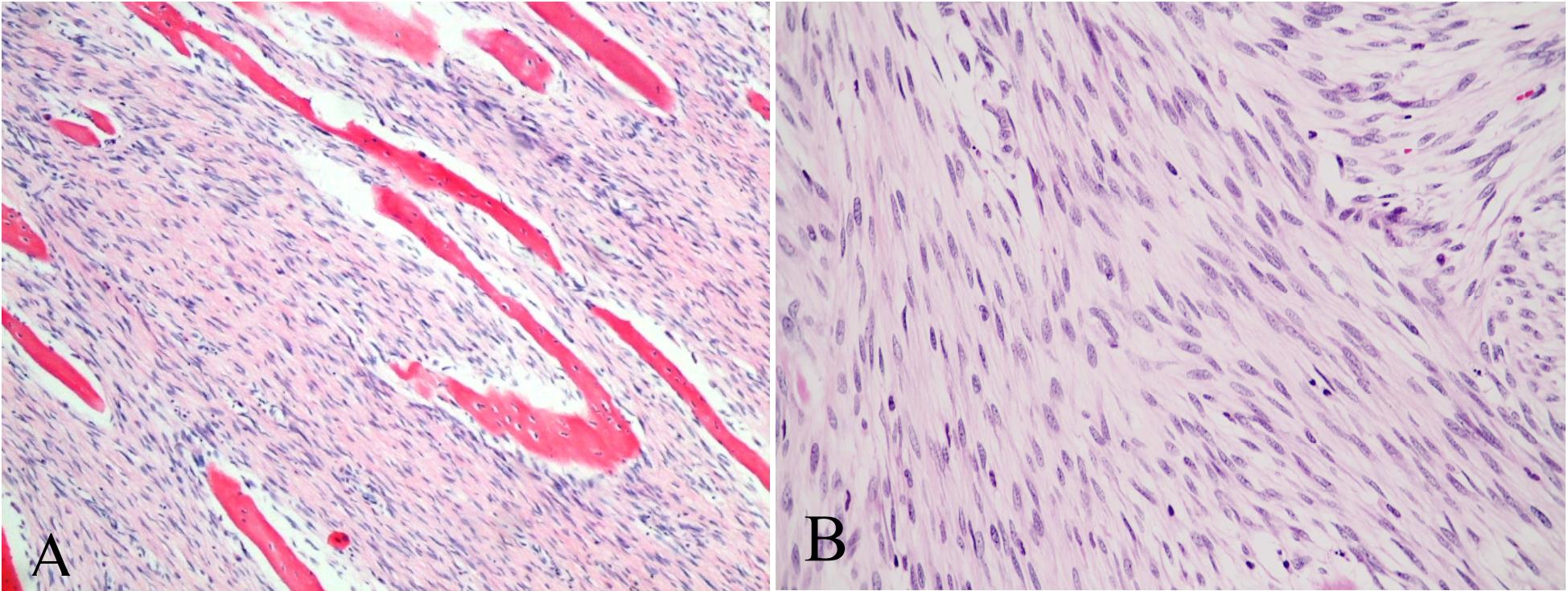
Figure 7. A. Well trabeculated bone interspersing with cellular spindle cell stroma. (H&E stained section at 200X magnification)
B. Mild nuclear atypia with rare to few mitotic figures. (H&E stained section at 400X magnification) (H&E stained section at 10X magnification)
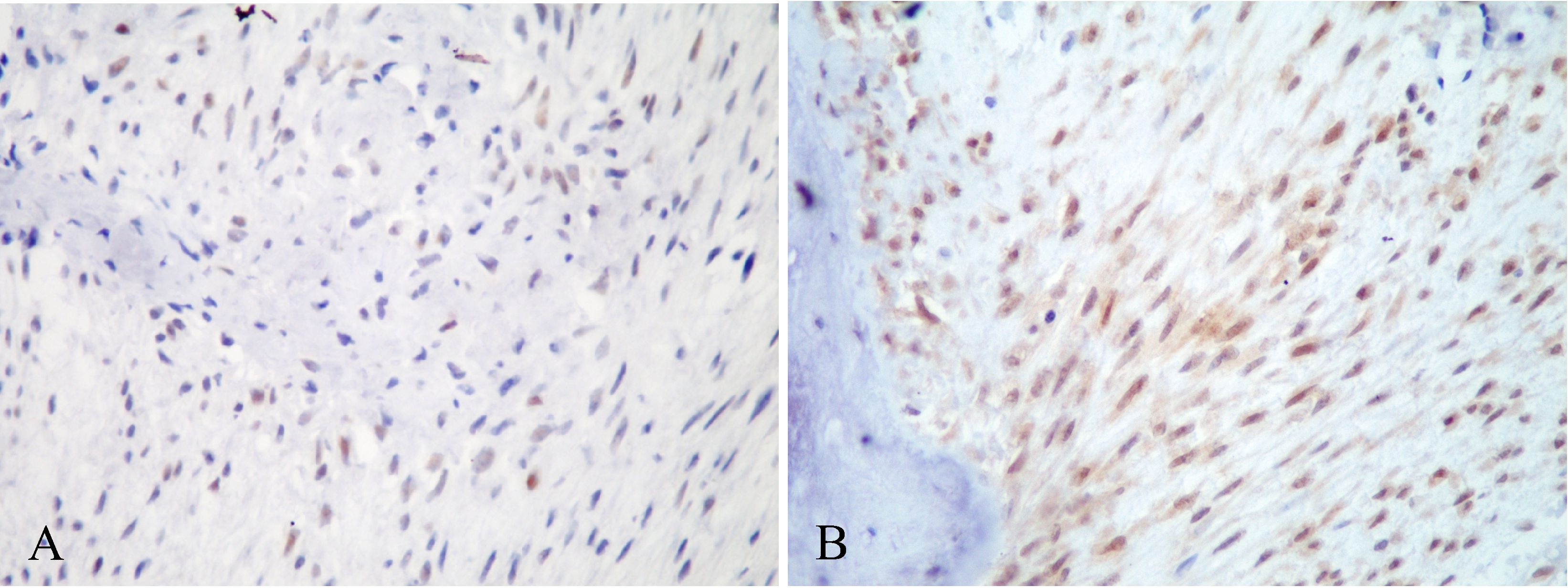
Figure 8. A. Focal nuclear staining of MDM2 was observed in tumor cells. (Immunohistochemical stained section at 400X magnification),
B. Diffuse nuclear staining of CDK4 in tumor cells. (Immunohistochemical stained section at 400X mamagnification)
LGCO has variable appearances on plain radiographs. The most frequent appearance is osteolytic pattern with varying amounts of thick and coarse trabeculations, followed respectively by a predominantly osteolytic pattern with a few thin and incomplete trabeculae, a densely sclerotic with a mixed osteolytic and osteosclerotic patterns (2, 3).
Differential radiologic diagnosis of LGCO includes benign fibro-osseous lesions: fibrous dysplasia, nonossifying fibroma, desmoplastic fibroma and conventional osteosarcoma. The presence of aggressive imaging features on plain radiographs such as cortical destruction, and aggressive-type periosteal reaction provides helpful clue for differentiation of LGCO from benign fibro-osseous lesions. However, almost one third of LGCO in a study of 90 cases did not show features of malignancy on plain radiographs (2). In contrast, CT and MRI are helpful in every instance in identifying cortical disruption and soft tissue component, which are the key characteristics of malignancy (2, 3). Our rare case of LGCO of the left ilium demonstrated such imaging features on both plain radiographs and MRI. In addition, mixed osteolytic-osteosclerotic radiographic pattern in our case was classified as the least common subtype of LGCO (2). Interestingly, there was another case of LGCO arising in the nearby rare location of sacral bone merely revealed a large well defined, expansile, mixed osteolytic-osteosclerotic lesion without cortical disruption or periosteal reaction (7).
By histologic examination, diagnosis can be particularly difficult on biopsy specimens when only the fibroblastic stroma is obtained without the osseous component. The differential diagnosis by histologic appearance includes fibrous dysplasia and conventional fibroblastic type osteosarcoma. The characteristic of LGCO in differential diagnosis from fibrous dysplasia is the permeative growth pattern against preexisting host bone (4). In contrast to the conventional high grade fibroblastic osteosarcoma, spindle cells in LGCO often show bland nuclei or mild nuclear atypia with absence or presence of minimal mitotic figures. The key factors in differential diagnosis of LGCO from benign fibrous or fibro-osseous lesions of bone are the presence of cortical disruption and soft tissue extension (2, 3, 4). Immunohistochemical stains for MDM2 and CDK4 were shown to be sensitive and specific markers for the diagnosis of LGCO, and helped distinguish LGCO from other benign fibrous or fibro-osseous lesions of bone (6). Similar to other low grade sarcoma, dedifferentiation of LGCO cases has been reported in majority of the recurrent tumor and 10-36% of primary LGCO (1, 5, 8, 9). Interestingly, dedifferentiated component of LGCO also demonstrated positivity to MDM2 and CDK4 immunostaining, confirming the value of these markers for aiding the diagnosis of LGCO (9).
Concerning our LGCO case, we did not observe high grade component by histologic examination of the resected specimen and all surgical margins were free from tumor. This patient was not placed on neither radiotherapy nor chemotherapy after acknowledgement of the report of LGCO. However, he developed pulmonary metastasis finally. As far as we knew of the incubation period between tumor resection and metastasis was less than three years which seemed to be shorter than those reported cases (1, 5, 8, 9 ). However, the clinical course of the present case was quite similar to a case having lesion at similar site reported by Malhas et al ( 10 ): the patient developed recurrences and finally pulmonary metastasis 15 months after enbloc resection of ilial bone with reconstruction of fibula grafts. Since cases at this location were still scarce, it may be difficult to deduce as to whether pelvic lesions have worse prognosis than those of extremities. However, it is noteworthy to address.
In summary, we described a case of LGCO arising in a rare location of ilium with comprehensive imaging illustrations. LGCO is a rare subtype of osteosarcoma which can be histologically misdiagnosed as other benign or malignant bone lesions. The awareness of this entity should lead to avoid the over and under treatment.
References
1. Unni KK, Dahlin DC, McLeod RA, Pritchard DJ. Intraosseous well-differentiated osteosarcoma. Cancer. 1977; 40:1337-1347.
2. Andresen KJ, Sundaram M, Unni KK, Sim FH. Imaging features of low-grade central osteosarcoma of the long bones and pelvis. Skeletal Radiol. 2004; 33:373-379.
3. Yarmish G, Klein MJ, Landa J, Lefkowitz RA, Hwang S. Imaging characteristics of primary osteosarcoma: nonconventional subtypes. Radiographics. 2010; 30:1653-1672.
4. Vasiliadis HS, Arnaoutoglou C, Plakoutsis S, Doukas M, Batistatou A, Xenakis TA. Low-grade central osteosarcoma of distal femur, resembling fibrous dysplasia. World J.Orthop. 2013; 4: 327-332.
5. Schwab JH, Antonescu CR, Athanasian EA, Boland PJ, Healey JH, and Morris CD. A Comparison of Intramedullary and Juxtacortical Lowgrade Osteogenic Sarcoma. Clin. Orthop. Relat. Res. 2008; 466: 1318–1322.
6. Dujardin F, Binh MB, Bouvier C, Gomez-Brouchet A, Larousserie F, Muret Ad, Louis-Brennetot C, Aurias A, Coindre JM, Guillou L,Pedeutour F, Duval H, Collin C, de Pinieux G. MDM2 and CDK4 immunohistochemistry is avaluable tool in the differential diagnosis of lowgrade osteosarcomas and other primary fibro-osseous lesions of the bone. Modern Pathology 2011; 24: 624–637.
7. Liuhong W, Minming Z. Welldifferentiated intraosseous osteosarcoma in the sacrum: a case report. Iran J. Radiol. 2013; 10:175-178.
8. Righi A, Paioli A, Dei Tos AP, Gambarotti M, Palmerini E, Cesari M, Marchesi E, Donati DM, Picci P, Ferrari S. High-grade focal areas in low-grade central osteosarcoma: highgrade or still low-grade osteosarcoma? Clin. Sarcoma Res. 2010; 5:23
9. Yoshida A, Ushiku T, Motoi T, Beppu Y, Fukayama M, Tsuda H, Shibata T. MDM2 and CDK4 immunehistochemical coexpression in highgrade osteosarcoma: correlation with a dedifferentiated subtype. Am. J. Surg. Pathol. 2012; 36: 423–431.
10. Malhas AM, Sumathi VP, James SL, Menna C, Carter SR, Tillman RM, Leys L, Grimer RJ. Low-grade central osteosarcoma: a difficult condition to diagnose. Sarcoma. 2012; article ID 764797, 7 pages; http://dx.doi.org/10.1155/2012/76479


