Diagnostic accuracy of fine needle aspiration cytology of salivary glands
Kanchana Amornpichetkul, M.D., Khwananong Atthakettaworn, M.D.
Department of Pathology, Faculty of Medicine Siriraj Hospital,
Mahidol University, Bangkok 1070. Thailand.
ABSTRACT
Fine needle aspiration (FNA) cytology of suspected salivary gland lesions has an established role in preoperative diagnosis and management of patients. However diverse morphological patterns and overlapping features make it a challenging job, to give a precise diagnosis, at times. The aim of the present study is to investigate the accuracy of FNA cytology of salivary gland lesions by correlation between histology and cytology. One hundred salivary gland FNA specimens collected during 2002 - 2008 from 100 patients were reviewed and correlated with histopathology findings. Considering the results of histopathology as the diagnostic standard, the sensitivity, specificity, and accuracy of FNA cytology in diagnosis were 67, 100, and 96%, respectively. This study demonstrated that FNA cytology of the salivary gland is an effective and useful technique for diagnosis of salivary gland lesions. Accuracy depends on experience of both pathologists who interpret the specimens and surgeons and clinicians who perform the FNA.
Keywords: cytopathology, fine-needle aspiration, salivary gland
INTRODUCTION
Fine-needle aspiration (FNA) cytology is a widely used, safe, and relatively nontraumatic procedure that can quickly provide important information. The main goal of FNA of salivary gland lesions is to assist the clinician in the management of patients, who present with mass lesion.[1-3] Cytological examination aims to determine, whether a process is inflammatory or reactive, whether neoplasm is benign or malignant, and if possible aims to render a specific diagnosis. It has been argued that in the area of salivary gland tumors, surgical management relies less heavily on a specific preoperative diagnosis because almost all neoplastic salivary gland lesions will undergo surgical excision. However, knowing beforehand whether a lesion is malignant or benign will assist in preoperative planning and may prompt or postpone decisions for surgical intervention.
MATERIAL AND METHOD
The study samples are recruited from fine needle aspiration cytology of salivary gland lesions in Department of Pathology Siriraj Hospital during 2002-2008. This retrospective study consisted of100 FNA specimens of salivary glands obtained from the archives of the cytology laboratory, which were verified by pathologic diagnosis. The FNA cytologic results were classified into three diagnostic categories: benign, suspicion of malignancy, and malignant.
All 100 fine needle aspiration cytology specimens of salivary gland lesions were reviewed and correlated with histopathologic findings and analyzed.
STATISTICAL ANALYSIS
The sensitivity, specificity, and accuracy of FNA cytology were calculated using standard statistical methods.
RESULTS
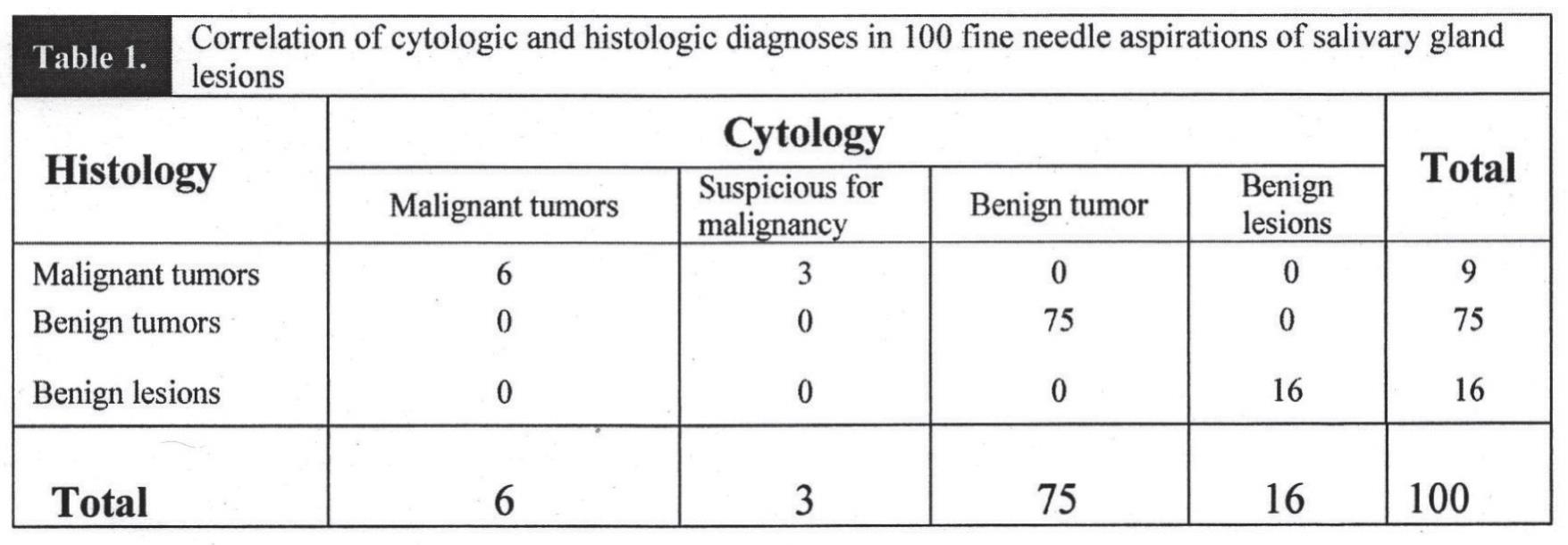
Histologic diagnoses following to Armed Forces Institute of Pathology (AFIP) and World Health Organization Classification of Tumors (WHO) [4, 5] were available in 100 cases. Of the 100 cases, 74% were from parotid glands, 24% were from submandibular glands. There were 53 females and 47 males, with a female: male ratio of 1.1:1. The age range was between 13-78 years. In our series, the overall sensitivity and specificity were 67% (6/9) and 100% (75/75), respectively. Table 1 shows the correlation between FNA cytology results and their histological diagnoses.
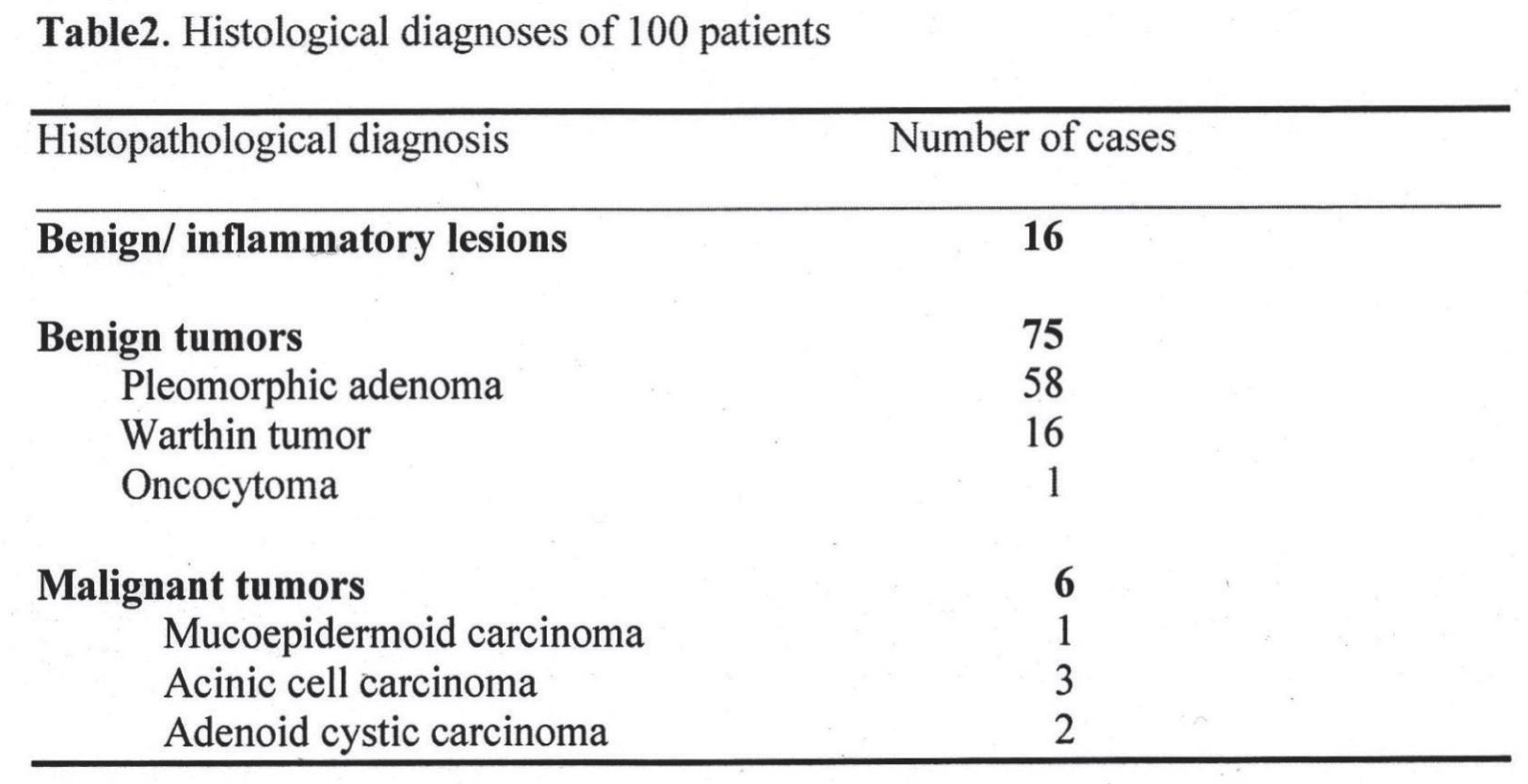
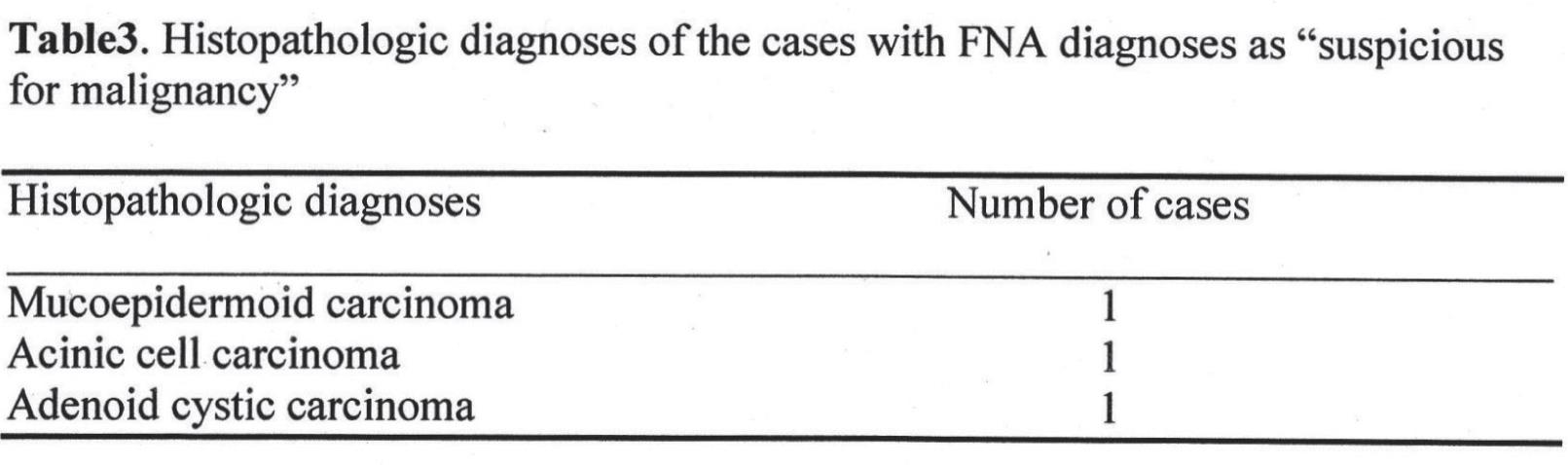
Table 2 shows the results of histological confirmation in 100 patients. Pleomorphic adenoma was the most common diagnosis. It consisted 58 % of all the benign lesions. The histological diagnoses of “suspicious for malignancy” cases were demonstrated in Table 3
DISCUSSION
The main goal of FNA is to determine if a mass is inflammatory and/or reactive, benign or malignant neoplasm and if possible, to render a specific diagnosis. The preoperative information concerning the tumor type can be informative to plan the best surgical approach. Close cooperation between the clinician and an experienced cytopathologist provides good outcome in FNA procedure. [3, 6, 7]
In our series, there was no any false positive case. There were a number of studies indicating unusual or atypical features and pitfalls that may cause difficulties in interpretation. The sensitivity, specificity, and diagnostic accuracy in our study were 67%, 100%, and 96%. Our results were similar to the previous report regarding salivary lesions, except that sensitivity in our study is lower their reports due to small number of malignant neoplasm samples.
FNA in salivary gland lesions is one of the most difficult areas in cytopathology due to the overlapping morphologic patterns in many benign and malignant salivary neoplasm.[2, 3, 6, 7] Besides that, histological patterns may show various differences within the same tumor. We reviewed three cases with “mucoepicermoid carcinoma”, and “acinic cell carcinoma” which were interpreted as “suspicious for malignancy” with FNA.
The cytologic diagnosis of mucoepidermoid carcinoma is difficult because an accurate diagnosis depends on adequate sampling and recognition of the mixed population of mucin-producing, intermediate, and epidermoid cells. Mucoepidermoid carcinomas are cystic, they may be difficult to distinguish from mucous retention cysts or Warthin tumors. [1-3, 8] Aspirates from adenoid cystic carcinoma usually yield moderately cellular smears with two components: epithelial cells and cellular basement membrane material, the latter appearing as homogeneous spherical structures that are diagnosis and nearly unique to this tumor. In hypocellular smears, the small and rather uniform tumor cells will make false negative result.[1, 3, 7, 9, 10]
Well-differentiated acinic cell carcinomas can be confused with nonneoplastic acinar tissue because of the similar appearance of the individual cells. It is one reason for “suspicious for malignancy” in our study.[1, 7, 9]
Distinction is possible by recognizing the ground-glass or vacuolated appearance of the acinic cell carcinomas instead of the purely granular appearance of the oncocytic neoplasm.[1, 3, 7, 9] Unfortunately, oncocytomas or Warthin tumors could not be excluded in our study, so it was interpreted as “suspicious for malignancy” with FNA.
CONCLUSION
FNA cytology of salivary gland masses is a valuable diagnostic method. Accuracy depends on experience of both pathologists who interpret the specimens and surgeon and clinician who perform the FNA. It is a widely used, safe, and relatively nontraumatic procedure that can quickly provide important information. The main goal of FNA of slivary gland lesions is to assist the clinician(s) in the management of patients, who present with superficial neck mass lesion. From this study, the results of sensitivity, specificity, and diagnostic accuracy are similar to the other reports and reveal high specificity and diagnostic accuracy (67, 100, and 96%, respectively). So, this method provides superior advantages for the clinicians and the patients.
REFERENCE
1. Leopold G, Koss R, Myron R. Koss’ diagnostic cytology and its histopathologic bases. 5th ed. Philadelphia: Pennsylvania; 1992.
2. Lim CM, They J, Loh KS, Chao SS, Lim LH, Tan LK.Role of needle aspiration cytology in the evaluation of parotid tumours. ANZ J Surg, 2007. 77(9): 742-4.
3. Rajwanshi A, Gupta K, Gupta N, Shukla R, Srinivasan R, Nijhawan R, et al. Fine-needle aspiration cytology of salivary glands: diagnostic pitfalls revisited. Diagn Cytopathol, 2006. 34(8): 580-4.
4. Barnes L, Eveson JW, Reichart P, Sidransky D. World health organization classification of tumours, Pathology and genetics of head and neck tumours. IARC Press. Lyon; 2005.
5. Gary L, Ellis L, Paul L. Auclair: Atlas of tumor pathology; tumors of the salivary glands. Armed Forces Institute of Pathology Washinton, D.C.;1995.
6. Elagoz S, Gulluoglu M, Yilmazbayhan D, Ozer H, Arslan I. The value of fine-needle aspiration cytology in salivary gland lesions, 1994-2004. ORL J Otorhinolaryngol Relat Spec, 2007. 69(1):51-6.
7. Orell SR. Pitfalls in fine needle aspiration cytology. Cytopathology, 2003. 14(4): 173-82.
8. Flezar M, Pogacnik A.Warthin’s tumour: unusual vs. common morphological findings in fine needle aspiration biopsies. Cytopathology, 2002. 13(4): 232-41.
9. Kumar V, Abbas AK, Fausto N. Robbins and cotran pathologic basis of disease. 7th ed Phila-delphia.Elsevier Saunders; 2005.
10. Paksoy N. A swelling in the submandibular gland: diagnostic pitfall. Cytopathology, 2007. 18(1): 52-5.


