Advantage of frozen section in management of thyroid nodule with preoperative fine needle aspiration in Siriraj Hospital,Bangkok, Thailand
Thiraphon Boonyaarunnate, M.D. and Kanchana Amornpichetkul, M.D
Department of Pathology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Kanchana Amornpichetkul
Department of Pathology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, 10700, Thailand
Email: Kanchana.amo@mahidol.ac.th
Abstract
Objectives: We aimed to evaluate the role of frozen section (FS) and preoperative fine-needle aspiration cytology (FNA) in thyroid nodular lesions.
Material and Methods: Sixty patients who underwent thyroidectomy with preoperative FNA and intraoperative FS were reviewed. The results were compared with the final histologic diagnosis (FHD) to assess their effectiveness in prediction of malignancy.
Results: The sensitivity and specificity of FNA were 56% and 100%, respectively and of FS were 88% and 100%, respectively. FNA revealed 34 benign, 16 indeterminate and 10 malignant lesions. All of malignant nodules in FNA were proved to be malignant in both FS and FHD: thirty-two lesions of benign FNA category were agreed with the result in FHD whereas two lesions were diagnosed as malignant and one of them was also diagnosed as malignancy by FS. Six out of 16 lesions of indeterminate FNA category were proved to be malignant in FHD and four of them were also diagnosed as malignancy by FS.
Conclusions: FS appears to give benefit when the results of FNA are indeterminate or benign. FS may not be necessary in the cases of malignant FNA results.
Keywords: Fine needle aspiration cytology; Frozen section; Thyroid
Introduction
Thyroid nodules are common with the prevalence of 4% to 7% in the general population. Most of them are benign but approximately 5% are malignant. Thyroid cancer is the most common endocrine malignancy and causes 26,000 deaths per year1. According to Siriraj Cancer Center annual statistical report 2004, it revealed that the incidence of thyroid cancer is 2.57% from all cancers and becomes the eighth most common malignancy (3.49%) in Thai female patients2. The clinical history and physical examination are the cornerstones of diagnostic clues in evaluation of the patient with thyroid nodules.
Fine needle aspiration (FNA) provides the most direct and specific informations for thyroid nodule. It can be performed at outpatient clinic and is relatively inexpensive. FNA is currently regarded as the test of choice for the diagnosis and management of the thyroid nodules. Although, up to 30% of the results are reported as suspicious or follicular lesions (indeterminate lesion). For the follicular lesion, cytology is unable to differentiate malignancy from benign aspirates3. According to the previous study, the prevalence of malignancy in patients who had thyroidectomy was 42%3. The sensitivity of FNA was 50- 92% and specificity was 45-99%4-7, 15.
The utility of intraoperative frozen section (FS) of thyroid gland remains controversial. Prolonged operating time and additional procedure cost are important constraint of FS. Literature review showed both extreme ends of the FS usage in management of thyroid nodules. Most authors used the intraoperative FS in the indeterminate cytologic result4, 5 9. The indeterminate result includes the so-called “follicular lesion” or “follicular neoplasm”, which can be hyperplastic nodules, follicular adenoma, or follicular carcinoma. But some authors believed that FS is only indicated in the cases of preoperative FNA of the thyroid nodules suggestive of malignancy and in order to determine the extent of the operation8. But one study concluded that preoperative FNA has no benefit in the selection of the surgical procedure and the intraoperative FS yields only little benefit for surgical management6.
This study was aimed to determine the necessity of FS for thyroid nodule when preoperative FNA is available.
MATERIAL AND METHODS
Sixty patients underwent thyroidectomy with both preoperative FNA and intraoperative FS at Siriraj Hospital, from January 2002 to December 2004. The cases with all three materials were included in this retrospective review. The patients with inadequate preoperative FNA were excluded from the study. The adequacy of cytologic specimen was defined by the presence of at least six clusters of 10 well-preserved follicular cells in each group or any material that contains abundant colloid.10, 12 All adequate materials were reviewed.
The preoperative FNA specimens were classified into one of the following categories: 1, benign; which includes nodular goiter, thyroid hyperplasia (Graves disease), lymphocytic/autoim-mune thyroiditis (Hashimoto thyroiditis), granulomatous thyroiditis (De Quervain thyroiditis); 2, malignant, including papillary carcinoma, medullary carcinoma, poorly differentiated (insular) carcinoma, undifferentiated (anaplastic) carcinoma, malignant lymphoma; 3,indeterminate lesion; follicular lesion (including oncocytic lesion); favor nodular goiter and favor follicular neoplasm, and suspicious lesion of papillary carcinoma. The FS specimens were categorized as follow: 1, benign; including nodular goiter, thyroid hyperplasia (Graves disease), thyroiditis, lymphocytic/autoimmune thyroiditis (Hashimoto thyroiditis), granulomatous thyroiditis (De Quervain thyroiditis); 2, malignant, including papillary carcinoma, follicular carcinoma (widely invasive), poorly differentiated (insular) carcinoma, undifferentiated (anaplastic) carcinoma, malignant lymphoma, medullary carcinoma; 3,indeterminate or follicular lesion (including oncocytic lesion); favor nodular goiter and favor follicular neoplasm.
The intraoperative cytology (IC) was undertaken and included in the study. The IC was categorized similarly to that of the preoperative FNA specimens. The intraoperative diagnosis was concluded from both FS and IC. All final histologic diagnoses (FHD) were performed based on WHO classification of endocrine organs 2004 for neoplastic lesion and AFIP 1992 for non-neoplastic lesion12,13.
The sensitivity, specificity, accuracy, positive predictive value and negative predictive value of the FNA and FS were assessed by using FHD as gold standard. Weighted kappa coefficient was used to determine the degree of agreement between FNA and FS diagnoses
RESULTS
Patient age was 46.75 ± 15.5 years (range 16-80 years). Of the 60 patients, 54 (90%) were female and 6 (10%) were male. Thirty percents of all cases were malignant. Comparison of final histologic diagnoses between male and female was reported in Table 1. The benign group (n=42) was composed of 5 males (11.9%) and 37 females (88.1%). The malignant group (n=18) was composed of 1 male (5.6%) and 17 females (94.4%). Male accounted for 83.3% in benign group and 16.7% in malignant group whereas female 68.5% in benign and 31.5% in malignant groups. The final histologic diagnosis was shown in Table 2.
Table 1 Comparison of histologic diagnoses between male and female
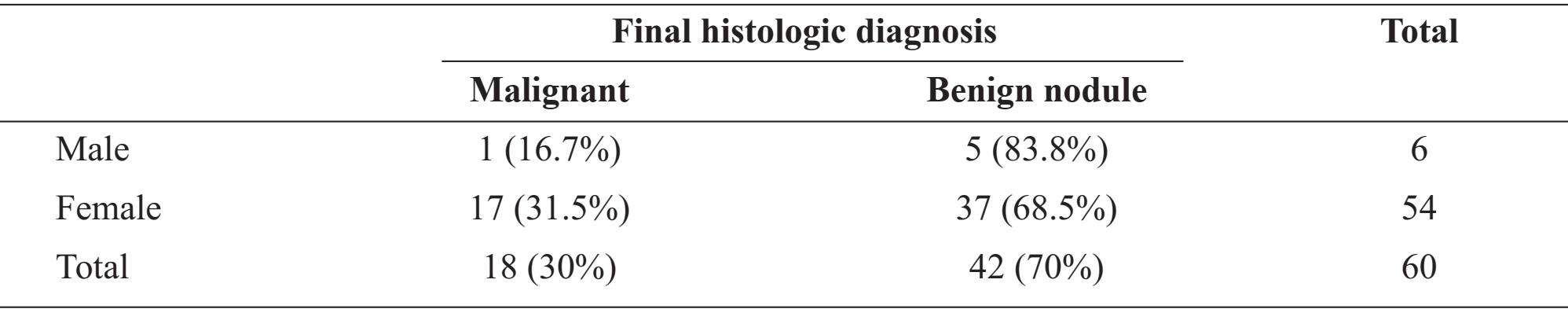
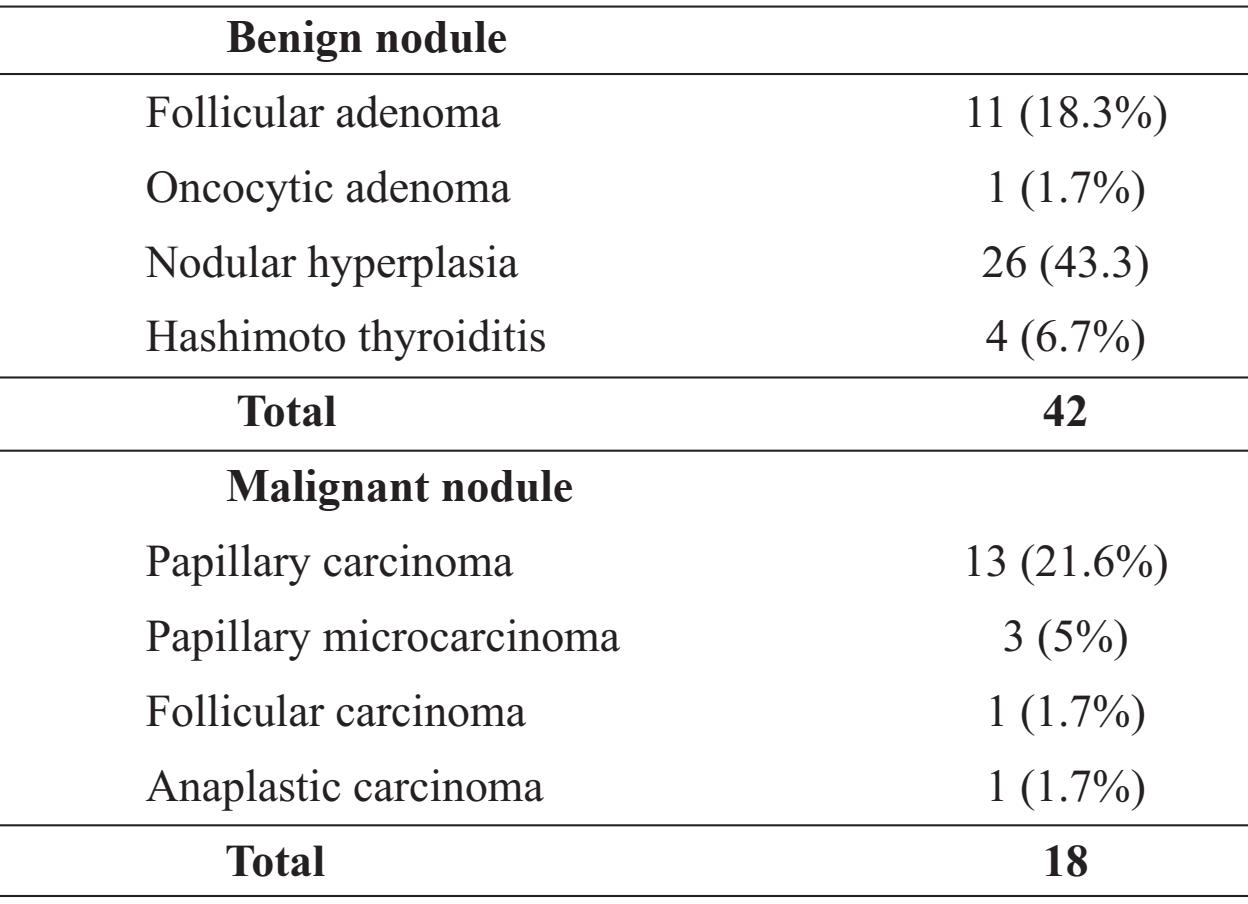
Table 2 Final histologic diagnosis
Comparison between FS and FHD
As in table 3, FS found 36 benign, 15 malignant and 9 indeterminate lesions. Thirty-four of 36 benign (94.4%) and all 15 malignant (100%) lesions were concordant with FHD. Two benign lesions diagnosed by FS were papillary microcarcinoma (small sized lesion) in FHD. One in 9 indeterminate lesions by FS as follicular lesion favoring neoplasm was proved to be follicular carcinoma in FHD. Sensitivity, specificity, accuracy, positive predictive value and negative predictive value of FS were 88%, 100%, 95%, 100% and 93% respectively.
Comparison between preoperative FNA and FHD
As in table 4, benign lesions were found in 34 cases while malignancy was diagnosed in 10 cases; 16 cases were indeterminate lesions. Thirty two (94.1%) out of 34 benign cases were agreed with FHD whereas two cases were proved as malignancy by FHD. One of these two cases was papillary microcarcinoma (0.8 cm. in diameter) and the other one papillary microcarcinoma (0.3 cm. in diameter) with extensive chronic lymphocytic thyroiditis. Six of indeterminate lesions (37.5%) were malignancy in FHD composing of 4 papillary carcinomas, 1 papillary microcarcinoma and 1 follicular carcinoma.
All of 10 malignant cases were concordant with FHD. In FNA, sensitivity, specificity, accuracy, positive predictive value and negative predictive value were 56%, 100%, 87%, 100% and 84% respectively.
Comparison among preoperative FNA, FS and FHD
As in table 5, two cases of 3 papillary microcarcinomas were diagnosed as benignancy in FS while FNA interpreted as benign and indeterminate results. The rest was papillary microcarcinoma with extensive chronic lymphocytic thyroiditis that FNA misinterpreted as Hashimoto thyroiditis while FS gave correct diagnosis. Follicular carcinoma was diagnosed as indeterminate result in both FNA and FS. Four of 16 (25%) indeterminate cases of FNA were diagnosed as papillary carcinoma in both FS and FHD.
Table 3 Comparison of diagnoses obtained by frozen section and final histologic diagnosis
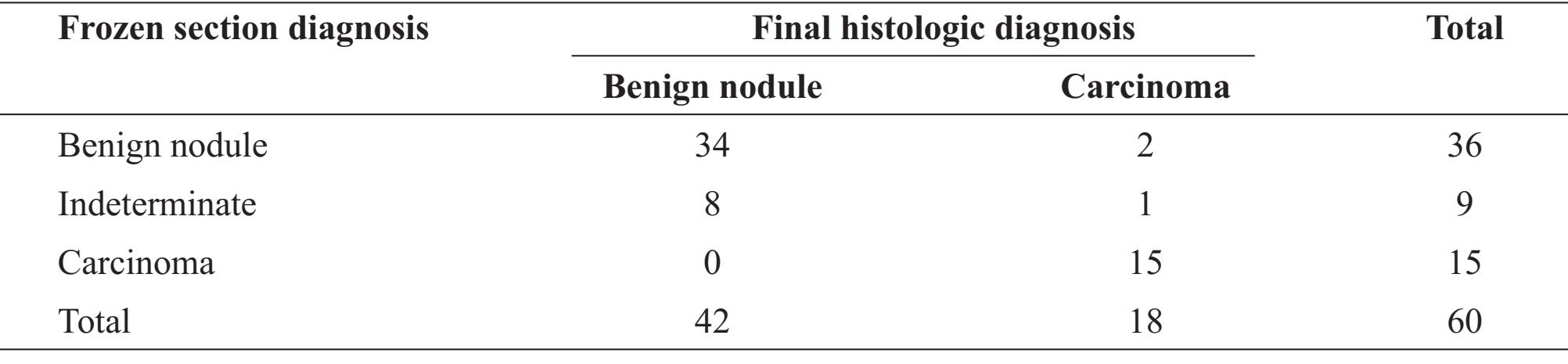
Table 4 Comparison of diagnoses obtained by fine needle aspiration and final histologic diagnosis
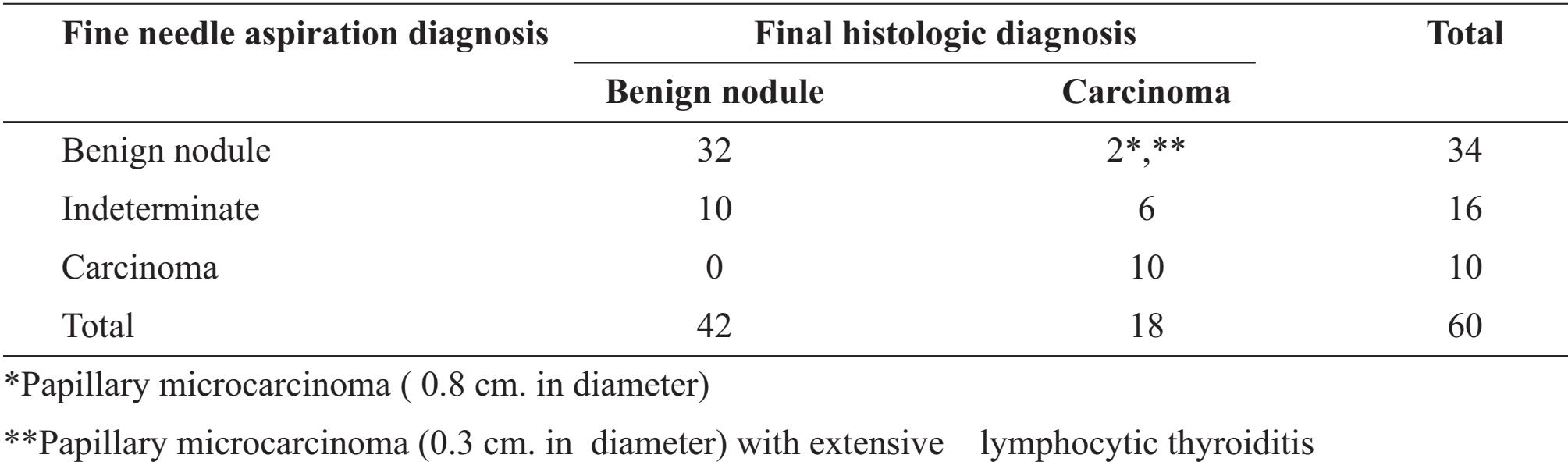
Table 5 Comparison of diagnoses obtained from fine needle aspiration, frozen section (FS) and final histologic diagnosis(FHD)
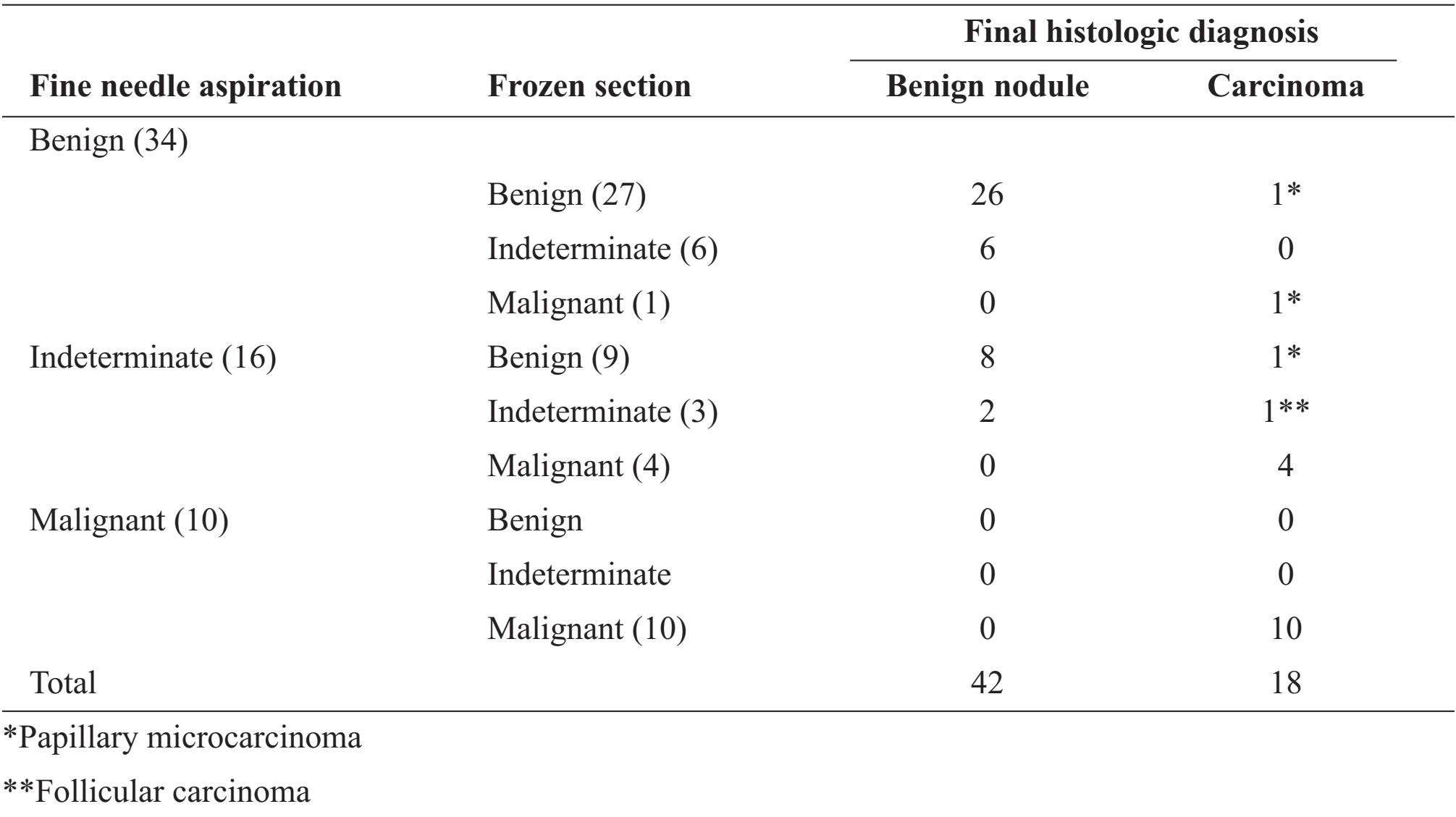
Indeterminate category of FNA in this study was subdivided into follicular lesion and suspicion of papillary carcinoma. Four cases of 13 follicular lesions were proved to be papillary carcinoma in FHD. In this group, FS detected 2 malignant cases (15.3%). Other two cases were papillary microcarcinoma and follicular carcinoma. Two out of 3 (66.7%) suspicious lesion of papillary carcinoma was confirmed by both FS and FHD. All of cases diagnosed as malignancy by FNA were concordant with FS and FHD. No false positive result was found in both FNA and FS. The kappa coefficient was 0.424 and implied that the FS diagnoses were moderate agreement with FNA diagnoses.
DISCUSSION
Diagnostic modalities for nodular thyroid lesion include radionuclide scanning, ultrasonography and fine needle aspiration cytology. FNA is currently regarded as the test of choice for the diagnosis and management of the thyroid nodules, thereby reducing the number and the extent of operative intervention performed.
In this study, sensitivity, specificity and accuracy of FNA were 56%, 100%, and 87%, consistent with those in previous studies. The results of FS, sensitivity, specificity and accuracy were 88%, 100% and 95%, respectively and consistent with those obtained from several literatures regarding FS for thyroid nodules4-7, 15.
The recent study of Tzu-Chieh Chao et. al. suggested that there is no benefit of FS for benign FNA result14. In our study, 2 in 34 (5.9%) cases in benign group by FNA were malignant lesion in FHD. FS can detect malignant lesion in 1 (2.9%) of benign FNA results (Table 3). One case of papillary carcinoma diagnosed in FHD was previously diagnosed by FS as Hashimoto’s thyroiditis with extensive chronic inflammatory cell infiltration. These results suggested that FS showed less advantage for benign FNA lesion because of chances of sampling error. Thus, the FS in this circumstance may not provide benefit; on the other hand it may increase cost and turnaround time of the operation. Many authors suggested to categorize the atypical and follicular lesion in the same group. Because of both benign and malignant lesions showed similar cytologic appearance. The diagnosis of malignancy depends on the demonstration of capsular or vascular invasion which is demonstrable only in histological preparations12. In indeterminate group of this study, four cases of 13 follicular lesions were proved to be malignant in FHD. Two in 4 cases were detected as malignant in FS. Two of 3 (66.7%) suspicious lesions of papillary carcinoma were proved to be papillary carcinoma by both FS and FHD. Six in 16 (37.5 %) cases diagnosed as malignancy in FNA were interpreted as follicular lesion or suspicion of papillary carcinoma. The sensitivity, specificity and accuracy of FS in the cases with FNA results of indeterminate group were 66.7%, 100%, and 87.5%. These results revealed benefit of FS in case of indeterminate lesions in FNA. FS provides worthy information for determining the extension of operation.
On the other hand, some reports14-15 indicated benefit of FS in malignant cytologic results. All cases interpreted by FNA in our study as malignant lesions were concordant with both FS and FHD. Thus, FS did not show benefit in this condition.
In this study, follicular carcinoma was misdiagnosed in both FNA and FS. As the definition of follicular carcinoma12, complete histologic capsule evaluation is needed. Because of operating time is an important constraint of FS. Thus, the chance to detect follicular carcinoma in FS was lower than papillary carcinoma. We missed two cases of small sized papillary carcinoma by both FNA and FS and one case of papillary carcinoma with extensive chronic lymphocytic thyroiditis by FNA. This was likely due to the fact that FNA alone cannot access to a very small lesion (less than 10 mm. in diameter). FNA with adjunct imaging guidance should be more helpful in this small lesion. But this is not routinely used in the FNA of thyroid gland at Siriraj Hospital. However, it is fortunate that small sized papillary carcinomas often have benign behavior and good prognosis. It can be managed by lobectomy and thyroid suppression rather than total thyroidectomy16-19. Lobectomy was performed in two cases of small sized papillary carcinoma and total thyroidectomy was performed in one papillary carcinoma with extensive chronic lymphocytic thyroiditis. Thus, small sized carcinoma can give a major pitfall of FNA procedure.
The limitations of our study were 1) the quality of slide preparations varied upon different clinicians 2) small number of patients who had complete all three histologic modalities due to the fact that most cases of FNA in Siriraj Hospital were managed without operation. The prospective study with larger number of patients should be performed to confirm the advantages and disadvanges of FNA and FS in the management of thyroid disease.
CONCLUSION
FNA and FS are specific, accurate and sensitive diagnostic technique for evaluating nodular thyroid disease. Routine use of FS in all operative cases is not recommended. FS is useful when FNA interpreted as suspicion of papillary carcinoma and shows little benefit in benign FNA results. FS does not prove benefit when FNA interpreted as malignancy.
REFERENCES
1. Bernard W. Stewart and Paul Kleihues. World Cancer Report; International Agency for Research on Cancer, 2003; 257-260.
2. Siriraj Cancer Center, Faculty of Medicine Siriraj Hospital, Mahidol University. Tumour Registry: Statistical Report 2004. Bangkok: Siriraj Cancer Center, 2004.
3. Barbara Miller, Shelby Burkey, Guy Lindberg, et al. Prevalence of malignancy within cyto-logically indetermininate thyroid nodules. The American Journal of Surgery 2004; 188:459462.
4. Bassam Abboud, Soha Allam and Lara Abou Chacra, et al. Use of fine-needle aspiration cytology and frozen section in the management of nodular goiters. Head & Neck 2003; 5:32-36.
5. P. Caraci, S. Aversa, A. Mussa, et al. Role of fine- needle aspiration biopsy and frozen-section evaluation in the surgical management of thyroid nodules 2002; 89: 797-801.
6. Ari D.Brooks, Ashok R. Shaha, Wilson Du-Mornay, et al. Role of Fine-Needle Biopsy and Frozen Section Analysis in the Surgical Management of Thyroid Tumors 2001; 8(2): 92-100.
7. R. J. De Vos Nederveen Cappel, N. D. Bouvy, H. J. Bonjer, et al. Fine needle aspiration cytology of thyroid nodules: how accurate is it and what are the causes of discrepant cases? 2001 ; 12: 399-405
8. T. L. Chow, V. Venu and S. P. Y. Kwok. Use of fine-needle aspiration cytology and frozen section examination in diagnosis of thyroid nodules. ANZ J. Surg 1999; 69: 131-133.
9. Michael S. P. Cheng, Joanna L. Morgan and Jonathan W. Serpell. Does frozen section have a role in the intraoperative management of thyroid nodules? ANZ J. Surg 2002; 72 570-572.
10. Edmund S. Cibas, Barbara S. Ducatman. Cytology Diagnostic principles and clinical correlates second edition. Saunders, 2003.
11. Winifred Gray and Grace T. McKee. Diagnostic Cytopathology second edition. Churchill Livingstone, 2003.
12. Ronald A. DeLellis, Picardo V. Lloyd, Philipp U. Heitz, et al. WHO Classification of tumours: Pathology and Genetics of Tumours of Endocrine Organs. IARCPress, Lyon, 2004.
13. Juan Rosai, Maria Luisa Carcangiu, Ronald A. Delellis, et al. Atlas of tumor pathology: Tumors of the thyroid gland. Armed Forces Institute of Pathology, 1992.
14. Tzu-Chieh Chao, Jen-Der Lin, Hsiao-Hsiang Chao et al. Surgical treatment of solitary thyroid nodules via fine-needle aspiration biopsy and frozen section analysis. Ann Surg. Onco; 14(2): 712-718.
15. Richards ML, et al. Is thyroid frozen section too much for too little? Am J Surg 2002; 184: 510-4.
16. T J Stephenson. Prognostic and predictive factors in endocrine tumours. Histopathology 2006, 48, 629-643.
17. Leigh Delbridge. Solitary thyroid nodule; current management. ANZ J. Surg. 2006; 76: 381-6.
18. Cocks, H. C. A review of the evidence base for the management for thyroid disease. Clinical otolaryngology 2005; 30: 500-10.
19. Yusra Cheema, Sarah Olson Diane Elson, at el. What is the biology and optimal treatment for papillary microcarcinoma of the thyroid? Journal of Surgical Research 2006; 143: 160162.


